Метод получения трехмерных клеточных сфероидов: универсальный инструмент для изучения цитотоксических свойств противоопухолевых соединений in vitro
- Авторы: Согомонян А.С.1,2, Шипунова В.О.1,2,3,4, Соловьев В.Д.1,4, Ларионов В.И.1, Котельникова П.А.1,4, Деев С.М.1,2
-
Учреждения:
- Институт биоорганической химии им. академиков М.М. Шемякина и Ю.А. Овчинникова РАН
- Национальный исследовательский ядерный университет «МИФИ»
- Научно-технологический университет «Сириус»
- Московский физико-технический институт (национальный исследовательский университет)
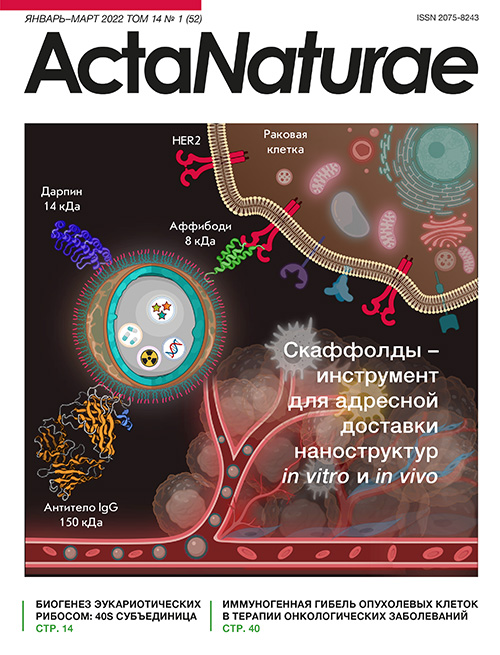
- Выпуск: Том 14, № 1 (2022)
- Страницы: 92-100
- Раздел: Экспериментальные статьи
- Дата подачи: 23.09.2021
- Дата принятия к публикации: 11.02.2022
- Дата публикации: 10.05.2022
- URL: https://actanaturae.ru/2075-8251/article/view/11603
- DOI: https://doi.org/10.32607/actanaturae.11603
- ID: 11603
Цитировать
Аннотация
Разработан метод 3D-культивирования клеток с образованием сфероидов для прогнозирования функциональной активности различных соединений in vivo. Для формирования и роста объемных клеточных сфероидов использовали агарозный гель, представляющий собой матрицу, состоящую из 9 низкоадгезивных U-образных микроячеек размером 2.3 × 3.3 мм, помещаемую в лунку 12-луночного планшета. Формы для заливки агарозного геля созданы методом 3D-печати. Эффективность метода показана на примере клеточной линии карциномы яичников человека SKOVip-kat со стабильной цитоплазматической экспрессией красного флуоресцентного белка Katushka и сверхэкспрессией мембраноассоциированного онкомаркера HER2. Сфероиды линии SKOVip-kat визуализированы методом флуоресцентной микроскопии. Концентрации клеток оптимизированы для формирования сфероидов с одинаковой формой, размером и плотными межклеточными контактами. Для валидации разработанной модели оценена цитотоксичность адресного анти-HER2 иммунотоксина на основе анти-HER2 каркасного белка DARP 9_29 и фрагмента экзотоксина Pseudomonas aerиginosa – DARP-LoPE – на 2D- и 3D-культурах клеток SKOVip-kat. Выявлено различие цитотоксических свойств DARP-LoPE в 2D- и 3D-культуре: значение IC50 в 3D-культуре на порядок выше, чем в монослойной культуре. Описан универсальный метод 3D-культивирования клеток млекопитающих на основе многоразовых форм для заливки агарозного геля, позволяющий воспроизводимо получать мультиклеточные сфероиды с плотными контактами для задач молекулярной и клеточной биологии.
Ключевые слова
Полный текст
СПИСОК СОКРАЩЕНИЙ МТТ – 3-(4,5-диметилтиазол-2-ил)-2,5-дифенилтетразолий бромид; ФИТЦ – флуоресцеин-5(6)-изотиоцианат; DARPin – белок с повторяющимися анкириновыми мотивами; LoPE – низкоиммуногенный участок экзотоксина А грамотрицательных бактерий Pseudomonas aeruginosa; HER2 – рецептор 2 эпидермального фактора роста человека.
ВВЕДЕНИЕ
Культивирование клеток млекопитающих в условиях in vitro остается одним из самых ценных инструментов молекулярной и клеточной биологии. В 1885 году Вильгельм Ру (Wilhelm Roux) разработал способ культивирования клеток, инкубируя живые клетки куриного эмбриона в физиологическом растворе в течение нескольких дней, а в 1906 году американский зоолог Росс Гранвилл Харрисон (Ross Granville Harrison) стал первым ученым, который вырастил искусственную культуру ткани [1]. Именно с конца 19 века культуры клеток стали применяться как инструмент для исследования взаимодействия различных веществ с живыми объектами [2]. Двумерные (2D) клеточные модели, являющиеся в настоящее время основным инструментом в экспериментах in vitro, находят широкое применение в фундаментальных и прикладных исследованиях, в частности, для разработки методов противоопухолевой терапии с использованием различных гибридных конструкций [3] или наночастиц с загрузкой активных веществ [4–9]. При исследованиях в 2D-культурах учитываются отличия от животных моделей in vivo, однако, чтобы спрогнозировать тот или иной эффект в организме, необходимо провести большое число экспериментов на клеточных культурах. К другим недостаткам монослойных культур относится отсутствие тканевой структуры и неограниченный доступ клеток к таким компонентам ростовой среды, как кислород, питательные вещества и метаболиты, в отличие от опухолевой ткани, где доступ этих веществ более вариабелен. Из-за таких ограничений появилась потребность в альтернативной системе, способной имитировать органы и позволяющей проводить рутинные эксперименты в большом количестве без привлечения лабораторных животных. Такими системами стали сферические скопления клеток с межклеточным взаимодействием – трехмерные (3D) модели [10], такие, как плотные скопления клеток, сфероиды, выращиваемые на поверхности низкоадгезивного пластика [11] или агарозы [12], а также полученные с использованием метода «висячих капель» [13], «альгинатных капсул» [14] и других трехмерных систем.
3D-сфероиды опухолевых клеток более приближены к in vivo моделям, чем 2D-культуры, которые не отражают архитектуру органов животных, имеющих специфическое строение и пространственную организацию. Сфероиды служат основой для создания органоидов и органов, которые имитируют гетерогенность и патофизиологию онкологических процессов в живом организме, они применяются для тестирования потенциальных лекарственных препаратов [11, 15, 16].
Известно, что опухолевая ткань состоит не только из раковых клеток, но и из стромальных клеток, таких, как фибробласты, эндотелиальные клетки сосудов, перициты, адипоциты, лимфатические эндотелиальные клетки и клетки иммунной системы. Эти клетки способствуют формированию и росту опухоли, а также участвуют в развитии устойчивости к противоопухолевым препаратам [17]. Сфероиды, состоящие только из опухолевых клеток, формируют взаимодействия клетка–клетка и клетка–внеклеточный матрикс и образуют тем самым барьер для исследуемых веществ [18]. Поэтому результаты исследований цитотоксических соединений на 3D-моделях отличаются от результатов в монослойных культурах. Таким образом, 3D-культуры наиболее подходят для in vitro исследований, направленных на прогнозирование и моделирование реакции опухоли на воздействие лекарственных препаратов. Следовательно, внедрение таких объектов в лабораторную практику сократит затраты и время на выявление новых лекарственных препаратов-кандидатов, а также ускорит процесс клинических испытаний, сократив время до выхода на фармакологический рынок [18, 19].
В данной работе представлен простой и универсальный метод создания 3D-сфероидов – скоплений клеток одинаковой формы и размера – для изучения активности веществ как в фундаментальных, так и в доклинических исследованиях. С помощью 3D-печати получены формы для заливки гелей – молды – из фотополимерной смолы. В молды заливали агарозу, которая служила основой для лунок, где формируются клеточные сфероиды. Методом флуоресцентной микроскопии показано наличие большого количества живых клеток, которые превалируют над мертвыми при росте сфероида. При сравнении 2D- и 3D-клеточных культур выявлены существенные различия в цитотоксичности оригинального адресного иммунотоксина DARP-LoPE [20]. Так, значение IC50 данного иммунотоксина в 3D-культуре примерно на порядок выше, чем в 2D, что необходимо учитывать при подборе доз препарата при инъекции in vivo в терапевтических целях.
ЭКСПЕРИМЕНТАЛЬНАЯ ЧАСТЬ
Условия культивирования клеточных линий
Флуоресцентная клеточная линия карциномы яичников SKOVip-kat получена ранее для исследования действия противоопухолевых соединений на внутрибрюшинную модель метастазирующего рака лабораторных животных с иммунодефицитом [20]. Клетки CHO получены из коллекции лаборатории молекулярной иммунологии ИБХ РАН. Клеточные линии SKOVip-kat и CHO культивировали в ростовой среде DMEM (Gibco, США) с 10% фетальной бычьей сыворотки (Capricorn, Германия) на культуральных флаконах (Nunc, Дания) в CO2-инкубаторе (BINDER, Германия) при 37°C и 5% CO2. С поверхности культуральных флаконов клетки снимали с помощью раствора Версена («ПанЭко», Россия).
Получение сфероидов флуоресцентной клеточной линии SKOVip-kat
Формы для заливки агарозы (молды) получали с использованием 3D-принтера FormLabs Form3 (США). Молды получали с использованием фотополимерной смолы FormLabs Grey Resin 1L (США). В качестве материала для форм, в которых будут формироваться сфероиды, использовали агарозу 1% («ПанЭко»), разведенную в ростовой бесцветной среде Fluorobrite DMEM (Gibco) без добавления фетальной бычьей сыворотки. Сфероиды получали, внося клеточную суспензию SKOVip-kat в лунки агарозного геля в 12-луночном планшете (Nunc) с ростовой средой DMEM (Gibco) с добавлением 10% фетальной бычьей сыворотки (Capricorn), и растили в течение 5 дней в CO2-инкубаторе (BINDER, Германия) при 37°C и 5% CO2. Образовавшиеся сфероиды окрашивали флуоресцентными красителями и получали изображения на флуоресцентных микроскопах Leica DMI6000B (Leica Microsystems, Германия) и Axiovert 200 (Carl Zeiss, Германия).
Флуоресцентная микроскопия
Для визуализации изображений использовали флуоресцентные красители Хёхст 33342 («ПанЭко»), пропидий йодид и акридиновый оранжевый (Sigma-Aldrich, США).
Окрашенные сфероиды SKOVip-kat визуализировали с помощью инвертированных флуоресцентных микроскопов Leica DMI6000B и Axiovert 200. Флуоресценцию белка Katushka (TurboFP635) возбуждали ртутной лампой HBO 100W флуоресцентного микроскопа Axiovert 200 c фильтрами возбуждения 565/30 нм и эмиссии 620/60 нм, Хёхст 33342 c фильтрами возбуждения 365/12 нм и эмиссии 397/LP нм, пропидий йодид c фильтрами возбуждения 565/30 нм и эмиссии 620/60 нм. Флуоресценцию белка Katushka возбуждали также металлической галогенидной лампой флуоресцентного микроскопа Leica DMI6000B c фильтрами возбуждения 545/30 нм и эмиссии 610/75 нм, Хёхст 33342 c фильтрами возбуждения 405/10 нм и эмиссии 460/40 нм, пропидий йодид c фильтрами возбуждения 545/30 нм и эмиссии 610/75 нм, акридиновый оранжевый c фильтрами возбуждения 470/40 нм и эмиссии 525/50 нм. Для визуализации 2D-клеточных линий SKOVip-kat и CHO использовали пластиковые 96-луночные планшеты (Nunc). Клетки инкубировали в 100 мкл ростовой бесцветной среды DMEM (Gibco) с фетальной бычьей сывороткой (Capricorn) в течение 12 ч при 37°C и 5% CO2. Затем вносили моноклональное антитело трастузумаб либо иммунотоксин DARP-LoPE, конъюгированные с флуоресцентным красителем флуоресцеин-5(6)-изотиоцианатом (ФИТЦ), в конечной концентрации 2 мкг/мл [7] и в объеме 100 мкл. Клетки отмывали от несвязавшихся белков и ресуспендировали в 1% растворе бычьего сывороточного альбумина в фосфатном буфере. Визуализацию проводили на флуоресцентном микроскопе Leica DMI6000B.
Анализ выживаемости клеточных линий
Цитотоксичность клеточных линий SKOVip-kat [20] и CHO, инкубированных с иммунотоксином DARP-LoPE [21], анализировали с помощью колориметрического МТТ-теста (МТТ – желтый тетразолиевый краситель, который восстанавливается в пурпурный формазан живыми клетками) [22].
Анализ проводили в 96-луночном планшете (Nunc). Клетки SKOVip-kat и CHO (3.5 × 103 клеток на лунку) инкубировали в 100 мкл ростовой бесцветной среды DMEM (Gibco (Thermo Scientific), США) с 10% фетальной бычьей сыворотки (Capricorn) в течение 12 ч при 37°C и 5% CO2. Далее добавляли 100 мкл иммунотоксина DARP-LoPE и инкубировали в течение 72 ч. После чего среду стряхивали, вносили 100 мкл МТТ в концентрации 0.5 г/л. Через 1 ч стряхивали раствор МТТ, в лунки вносили ДМСО в объеме 100 мкл (Panreac-AppliChem, США) для растворения формазана, после чего измеряли оптическую плотность на спектрофотометре Infinite M100 Pro (Tecan, Австрия) при длине волны λ = 570 нм и длине волны сравнения 630 нм. Значение концентрации иммунотоксина DARP-LoPE, вызывающее ингибирование роста 50% (IC50) клеток линий SKOVip-kat и CHO, определяли с помощью программного обеспечения GraphPad Prism 8.0.1.
РЕЗУЛЬТАТЫ И ОБСУЖДЕНИЕ
Цель нашей работы состояла в получении воспроизводимых in vitro 3D-сфероидов, имитирующих характеристики опухолевых тканей, для тестирования различных активных веществ, в том числе и лекарственных препаратов. Мы использовали линию клеток карциномы яичников человека SKOVip-kat, сверхэкспрессирующих на своей поверхности рецептор HER2 – диагностический и терапевтический маркер некоторых онкологических заболеваний. Эта клеточная линия получена ранее путем стабильной трансфекции клеток линии SKOV3-1ip геном красного флуоресцентного белка Katushka [23]. Возбуждение и эмиссия флуоресценции белка Katushka находятся в ближней инфракрасной области (588 и 635 нм) [24], входящей в «окно прозрачности биоткани», что позволяет с одинаковой эффективностью визуализировать данные клетки как in vitro, так и in vivo.
Формирование 3D-сфероидов с помощью агарозных форм
При формировании 3D-сфероидов за основу брали агарозу – биоразлагаемый, неадгезивный и нетоксичный природный полисахарид, полученный из морских водорослей [25]. Агароза обладает характеристиками, необходимыми для создания трехмерных моделей клеточных культур, такими, как большие поры (средний размер 100–300 нм), что позволяет обновлять питательные среды для 3D-роста клеток [25], а также обеспечивать доступ для газов и малых молекул [26]. Агароза является оптически прозрачным материалом, поэтому она удобна для микроскопической визуализации сфероидов. Агарозный гель застывает в молдах при комнатной температуре, что позволяет работать в стерильных условиях без существенных затруднений, при этом формируемые лунки геля доступны для наконечника пипетки, что позволяет вносить клетки или проводить другие манипуляции с формами.
Сформированные агарозные формы образуют 9 одинаковых лунок диаметром 2.3 мм и высотой 3.3 мм, в которых образуются сфероиды одинаковой величины и формы. Созданная форма представляет собой открытую систему, которая позволяет анализировать образование сфероидов и тестировать различные соединения с использованием методов световой и флуоресцентной микроскопии.
На рис. 1 представлена схема создания сфероидов клеточной линии SKOVip-kat. Молды для агарозного геля печатали на 3D-принтере FormLabs Form3 (США) с использованием фотополимерной смолы FormLabs Grey Resin (США). Вмещаемый объем агарозы в молде составил 1200 мкл, объем единичной агарозной лунки – 10 мкл. Поверхность агарозы неадгезивна для клеток, что приводит к самообразованию сфероида. Сфероиды формировались в течение 5 дней, что подтверждали визуально по наличию межклеточных контактов [26] (рис. 2). На рис. 2 представлены результаты оценки жизнеспособности клеток внутри сфероидов с помощью флуоресцентного микроскопа Leica DMI6000B. Для визуализации проводили съемку по оси Z с шагом 200 нм трех репрезентативных сфероидов, окрашенных флуоресцентными красителями. Флуоресцентный краситель акридиновый оранжевый окрашивает нуклеиновые кислоты живых клеток; пропидий йодид – нуклеиновые кислоты [27] мертвых клеток, так как мембраны живых клеток непроницаемы для красителя; Хёхст 33342 окрашивает нуклеиновые кислоты в ядрах [28] за счет прохождения через мембраны живых клеток [29]. Окрашивание акридиновым оранжевым и Хёхст 33342 показало, что живых клеток как внутри, так и снаружи сфероида больше, чем мертвых, окрашенных пропидий йодидом. Таким образом, полученные нами 3D-культуры клеток наиболее подходят для тестирования лекарственных препаратов, так как клетки в сфероиде создают межклеточные контакты и формируют приближенную модель раковых тканей, т.е. они представляют собой более адекватную in vitro систему в сравнении с 2D-культурами.
Рис. 1. Схема создания 3D-сфероидов клеток SKOVip-kat. В молды (формы для заливки геля) вносили раствор агарозы и оставляли гель застывать при комнатной температуре. В лунки застывшей формы вносили суспензию клеток SKOVip-kat. После формирования сфероидов клетки метили флуоресцентными красителями и анализировали методом флуоресцентной микроскопии
Рис. 2. Визуализация сфероидов SKOVip-kat. Визуализация трех сфероидов с шагом 200 нм по оси Z, окрашенных флуоресцентными красителями: акридиновым оранжевым, Хёхст 33342 и пропидий йодидом. Фильтры возбуждения и эмиссии для детекции акридинового оранжевого – 470/40 и 525/50 нм; пропидия йодида – 545/30 и 610/75 нм; Хёхст 33342 – 405/10 и 460/40 нм. Масштабная линейка 250 мкм
Оценка экспрессии рецептора HER2 на поверхности клеток SKOVip-kat
Рецептор HER2 (рецептор эпидермального фактора роста человека типа 2) – широко известный мембраноассоциированный онкомаркер [30–32]. Чаще всего этот рецептор сверхэкспрессируется при раке молочной железы, яичников, эндометрия, желудка и пищевода, при этом в нормальных клетках его экспрессия находится на низком уровне [33]. Например, этот онкомаркер находят в 30% случаев рака молочной железы [34], поэтому HER2 считается важной мишенью в диагностике и терапии опухолей. Экспрессию рецептора HER2 на поверхности клеток SKOVip-kat оценивали с использованием моноклонального антитела трастузумаб, конъюгированного с флуоресцентным красителем ФИТЦ. В качестве отрицательного контроля использовали клеточную линию CHO яичников китайского хомяка, на поверхности клеток которой отсутствует рецептор HER2 (рис. 3). Обе клеточные линии инкубировали с конъюгатом трастузумаб-ФИТЦ, а затем визуализировали на флуоресцентном микроскопе Leica DMI6000B. Данные, представленные на рис. 3, подтверждают присутствие рецептора HER2 на поверхности клеток SKOVip-kat.
Рис. 3. Визуализация экспрессии рецептора HER2 на клеточных линиях SKOVip-kat (HER2-положительные) и CHO (HER2-отрицательные) моноклональным антителом трастузумаб, конъюгированным с флуоресцентным красителем ФИТЦ. Экспрессия HER2 на поверхности клеток SKOVip-kat подтверждается интенсивным окрашиванием мембраны клеток анти-HER2-антителом. Ядра клеток окрашены Хёхст 33342. Фильтры возбуждения и эмиссии для детекции флуоресцентных красителей Хёхст 33342 – 405/10 и 460/40 нм, ФИТЦ – 470/40 и 525/50 нм. Масштабная линейка 50 мкм
Цитотоксичность иммунотоксина DARP-LoPE в 2D-культуре
Для валидации разработанной 3D-модели как средства изучения противоопухолевой эффективности соединений оценили цитотоксичность адресного противоопухолевого соединения – иммунотоксина DARP-LoPE.
Иммунотоксины – адресные белки, соединенные с токсином, выделенным из бактерий или ядовитых растений [35, 36], рассматриваются как одни из наиболее перспективных адресных молекул для онкотерапии. Иммунотоксин DARP-LoPE был сконструирован ранее генно-инженерным методом с использованием неиммуноглобулинового белка с анкириновыми повторами (Designed Ankyrin Repeat Proteins) DARP 9_29, который связывается с рецептором HER2 [37, 38], и низкоиммуногенного варианта участка экзотоксина А (LoPE), выделенного из грамотрицательных бактерий Pseudomonas aeruginosa [21]. Этот иммунотоксин специфично связывается с рецептором HER2 и вызывает гибель раковых клеток in vitro [21]. Более того, DARP-LoPE эффективно подавляет рост HER2-положительных ксенотрансплантатов карциномы яичников человека, что подтверждает эффективность адресных препаратов на основе дарпинов [5, 20, 21, 39].
На рис. 4 представлены результаты анализа цитотоксичности иммунотоксина DARP-LoPE и данные флуоресцентной микроскопии, подтверждающие специфичность связывания иммунотоксина с клетками SKOVip-kat. Цитотоксичность оценивали с помощью МТТ-теста и обрабатывали данные с использованием программного обеспечения OriginPro 2015. Полученные результаты указывают на адресную цитотоксичность иммунотоксина DARP-LoPE для клеточной линии SKOVip-kat и отсутствие цитотоксичности для CHO. Значение IC50 для иммунотоксина DARP-LoPE на клеточной линии SKOVip-kat составило 41.9 пМ (рис. 4А).
Визуализация опухолевых клеток с помощью мечения рецептора HER2 на поверхности клеточной линии SKOVip-kat моноклональным антителом трастузумаб и иммунотоксином DARP-LoPE, конъюгированным с ФИТЦ. Показано, что иммунотоксин эффективно взаимодействует с рецептором HER2 на поверхности опухолевых клеток, как и трастузумаб (рис. 4Б).
Рис. 4. Исследование взаимодействия адресного иммунотоксина DARP-LoPE с клетками SKOVip-kat.А – определение цитотоксичности DARP-LoPE по отношению к клеточным линиям SKOVip-kat и CHO методом МТТ-теста. За 100% принимали выживаемость клеток без взаимодействия с иммунотоксином DARP-LoPE.Б – визуализация живых клеток с помощью белка Katushka (TurboFP635) и красителя Хёхст 33342; визуализация экспрессии рецептора HER2 на клетках SKOVip-kat, инкубированных с моноклональным антителом трастузумаб-ФИТЦ и иммунотоксином DARP-LoPE-ФИТЦ. Фильтры возбуждения и эмиссии для детекции белка Katushka – 545/30 и 610/75 нм; флуоресцентных красителей: Хёхст 33342 – 405/10 и 460/40 нм и ФИТЦ – 470/40 и 525/50 нм. Масштабная линейка 50 мкм
Исследование цитотоксичности иммунотоксина DARP-LoPE в сфероидах SKOVip-kat
Для выбора оптимальных количеств клеток в лунках сфероидов тестировали диапазон концентраций от 1500 до 15000 клеток на лунку. Оптимальные концентрации определяли на 3-й день инкубации клеток в агарозных лунках по результатам микроскопии в проходящем свете и флуоресцентной визуализации белка Katushka в SKOVip-kat. Воспроизводимость результатов и формирование клеточных контактов (отсутствие разрозненности клеток) [26] наблюдали в лунках с 15000 клеток в сфероиде (рис. 5).
Рис. 5. Визуализация сфероидов SKOVip-kat и определение цитотоксичности иммунотоксина DARP-LoPE в 3D-культуре. Клетки инкубировали с различными концентрациями иммунотоксина и анализировали их жизнеспособность в течение 6 дней. Определяли цитотоксичность иммунотоксина DARP-LoPE по отношению к клеткам SKOVip-kat в 3D-культуре, при этом сфероиды формировали с разным количеством клеток SKOVip-kat. Показано, что для создания 3D-культуры оптимальным является 15000 клеток в сфероиде. Жизнеспособность клеток SKOVip-kat оценивали по флуоресценции белка Katushka с использованием флуоресцентной микроскопии в режиме реального времени на 3-й и 6-й день, при этом на 6-й день, инкубируя сфероиды с красителями. С помощью Хёхст 33342 визуализировали живые клетки, с помощью пропидия йодида – мертвые. Фильтры возбуждения и эмиссии для детекции Katushka – 565/30 и 620/60 нм; Хёхст 33342 – 365/12 и 397/LP нм и пропидия йодида –565/30 и 620/60 нм. Масштабная линейка 250 мкм
Вместе с подбором концентраций клеток изучали цитотоксичность иммунотоксина DARP-LoPE, инкубируя сфероиды с DARP-LoPE в различных концентрациях. После инкубации с белком и окрашивания Хёхст 33342 и пропидий йодидом образцы анализировали методом флуоресцентной микроскопии (рис. 5). Визуально определили IC50 иммунотоксина DARP-LoPE в 3D-культуре – 0.3 нМ, что примерно в 8 раз больше, чем IC50 в 2D-культуре – 41.9 пМ. Поскольку по структурной организации 3D-модели клеток более приближены к in vivo моделям животных, чем 2D, то результаты визуализации и определения цитотоксичности в трехмерной культуре, по-видимому, будут сопоставимыми с результатами, полученными на животных объектах in vivo.
ЗАКЛЮЧЕНИЕ
Переход от 2D- к 3D-моделям необходим из-за недостаточной информативности двумерных систем при исследовании различных эффектов или тестировании препаратов для диагностики и лечения различных заболеваний. Создание трехмерных сфероидов, имитирующих солидные опухоли, и внедрение их в исследовательскую практику необходимо и по этическим соображениям – результаты, полученные на таких системах, более приближены к результатам in vivo [40]. Таким образом, применение этих моделей, возможно, сократит количество экспериментов на животных, необходимых для скрининга лекарственных препаратов [41].
3D-сфероиды клеток образуют особую микросреду с отличающимися от двумерных структур характеристиками – значением pH, наличием и концентрацией аутокринных факторов, концентрацией кислорода и CO2; при этом клетки в таком микроокружении обладают своей морфологией, способностью к дифференцировке и пролиферации, а также реакцией на различные стимулы, тем самым имитируя поведение in vivo. Эти свойства клеток в сфероиде важны для исследования действия различных препаратов, так как созданная микросреда ограничивает их проникновение, поэтому для достижения желаемого эффекта требуется увеличенная концентрация вещества [18].
В нашей работе представлен метод создания сфероидов раковых клеток, основанный на 3D-печати молдов из фотополимерной смолы и их заливки агарозой. Это простой и воспроизводимый метод тестирования лекарственных препаратов, результаты определения цитотоксичности с его использованием будут более приближены к результатам in vivo. 3D-печать на сегодняшний день становится доступным методом получения форм с заданными характеристиками, который широко используется в разных областях, таких, как регенеративная медицина [42], инженерия [43], архитектура [44] и производство [45]. В настоящее время 3D-принтеры и материалы для создания желаемых объектов стали доступными по цене [46], что позволит использовать данную методику во многих лабораториях. Использование агарозы как основы для образования сфероидов делает этот метод максимально эффективным для рутинных экспериментов. Поскольку агароза низко адгезивна для клеток, то взаимодействия возникают только между клетками, что способствует росту клеток по всем направлениям, а не только в плоскости. Помимо этого, агароза – это прозрачный полимер, поэтому ее можно использовать в различных исследованиях, в частности, в фотодинамической терапии. Более того, разработанная модель сфероидов представляет собой открытую систему, в которой можно проводить такие манипуляции с клетками, как замена среды и отмывка от различных компонентов, внешние воздействия электромагнитным излучением, внесение клеток других типов (эндотелий, фибробласты), а также помещение образцов биоптата в единичную лунку.
На примере флуоресцентной клеточной линии SKOVip-kat с помощью разработанной методики получены воспроизводимые 3D-сфероиды одинаковой формы и размера. С использованием колориметрического теста и флуоресцентной микроскопии выявили значительные различия в действии адресного иммунотоксина на 2D- и 3D-модели. Таким образом, нами разработан простой и эффективный метод получения репрезентативных 3D-моделей сфероидов для молекулярно-биологических и клеточных исследований [47, 48].
Исследование выполнено при финансовой поддержке гранта РФФИ № 19-29-04012 мк (разработка 3D-модели ErbB2-положительных опухолей) и РНФ № 17-74-20146(выделение и очистка адресного иммунотоксина, определение цитотоксичности).
Об авторах
Анна Самвеловна Согомонян
Институт биоорганической химии им. академиков М.М. Шемякина и Ю.А. Овчинникова РАН; Национальный исследовательский ядерный университет «МИФИ»
Email: viktoriya.shipunova@phystech.edu
Россия, 117997, Москва; 115409, Москва
Виктория Олеговна Шипунова
Институт биоорганической химии им. академиков М.М. Шемякина и Ю.А. Овчинникова РАН; Национальный исследовательский ядерный университет «МИФИ»; Научно-технологический университет «Сириус»; Московский физико-технический институт (национальный исследовательский университет)
Автор, ответственный за переписку.
Email: viktoriya.shipunova@phystech.edu
Россия, 117997, Москва; 115409, Москва; 354340, Сочи; 141701, Долгопрудный
Владислав Денисович Соловьев
Институт биоорганической химии им. академиков М.М. Шемякина и Ю.А. Овчинникова РАН; Московский физико-технический институт (национальный исследовательский университет)
Email: viktoriya.shipunova@phystech.edu
Россия, 117997, Москва; 141701, Долгопрудный
Владислав Игоревич Ларионов
Институт биоорганической химии им. академиков М.М. Шемякина и Ю.А. Овчинникова РАН
Email: viktoriya.shipunova@phystech.edu
Россия, 117997, Москва
Полина Александровна Котельникова
Институт биоорганической химии им. академиков М.М. Шемякина и Ю.А. Овчинникова РАН; Московский физико-технический институт (национальный исследовательский университет)
Email: viktoriya.shipunova@phystech.edu
Россия, 117997, Москва; 141701, Долгопрудный
Сергей Михайлович Деев
Институт биоорганической химии им. академиков М.М. Шемякина и Ю.А. Овчинникова РАН; Национальный исследовательский ядерный университет «МИФИ»
Email: viktoriya.shipunova@phystech.edu
Россия, 117997, Москва; 115409, Москва
Список литературы
- Harrison R.G. // Exp. Biol. Med. 1906. V. 4. № 1. P. 140–143.
- Yao T., Asayama Y. // Reprod. Med. Biol. 2017. V. 16. № 2. P. 99–117.
- Grebenik E.A., Kostyuk A.B., Deyev S.M. // Russ. Chem. Rev. 2016. V. 85. № 12. P. 1277–1296.
- Shipunova V.O., Sogomonyan A.S., Zelepukin I.V., Nikitin M.P., Deyev S.M. // Molecules. 2021. V. 26. № 13. Р. 3955. doi: 10.3390/molecules26133955.
- Shramova E., Proshkina G., Shipunova V., Ryabova A., Kamyshinsky R., Konevega A., Schulga A., Konovalova E., Telegin G., Deyev S. // Cancers (Basel). 2020. V. 12. № 10. Р. 3014. doi: 10.3390/cancers12103014.
- Shipunova V.O., Komedchikova E.N., Kotelnikova P.A., Zelepukin I.V., Schulga A.A., Proshkina G.M., Shramova E.I., Kutscher H.L., Telegin G.B., Kabashin A.V., et al. // ACS Nano. 2020. V. 14. № 10. P. 12781–12795.
- Shipunova V.O., Kolesnikova O.A., Kotelnikova P.A., Soloviev V.D., Popov A.A., Proshkina G.M., Nikitin M.P., Deyev S.M. // ACS Omega. 2021. V. 6. № 24. P. 16000–16008.
- Zelepukin I.V., Popov A.A., Shipunova V.O., Tikhonowski G.V., Mirkasymov A.B., Popova-Kuznetsova E.A., Klimentov S.M., Kabashin A.V., Deyev S.M. // Mater. Sci. Eng. C. 2021. V. 120. P. 111717.
- Kabashin A.V., Kravets V.G., Wu F., Imaizumi S., Shipunova V.O., Deyev S.M., Grigorenko A.N. // Adv. Funct. Mater. 2019. V. 29. № 26. P. 1902692.
- Kapałczyńska M., Kolenda T., Przybyła W., Zajączkowska M., Teresiak A., Filas V., Ibbs M., Bliźniak R., Łuczewski Ł., Lamperska K. // Arch. Med. Sci. 2016. V. 14. № 4. P. 910–919.
- Zanoni M., Piccinini F., Arienti C., Zamagni A., Santi S., Polico R., Bevilacqua A., Tesei A. // Sci. Rep. 2016. V. 6. P. 19103.
- Liao W., Wang J., Xu J., You F., Pan M., Xu X., Weng J., Han X., Li S., Li Y., et al. // J. Tissue Eng. 2019. V. 10. Р. 2041731419889184. doi: 10.1177/2041731419889184.
- Białkowska K., Komorowski P., Bryszewska M., Miłowska K. // Int. J. Mol. Sci. 2020. V. 21. № 17. Р. 6225. doi: 10.3390/ijms21176225.
- Andersen T., Auk-Emblem P., Dornish M. // Microarrays. 2015. V. 4. № 2. P. 133–161.
- Zhang C., Yang Z., Dong D.-L., Jang T.-S., Knowles J.C., Kim H.-W., Jin G.-Z., Xuan Y. // J. Tissue Eng. 2020. V. 11. P. 1–17.
- Balalaeva I.V., Sokolova E.A., Puzhikhina A.D., Brilkina A.A., Deyev S.M. // Acta Naturae. 2017. V. 9. № 1. P. 38–44.
- Zanoni M., Cortesi M., Zamagni A., Arienti C., Pignatta S., Tesei A. // J. Hematol. Oncol. 2020. V. 13. № 1. P. 97.
- Sant S., Johnston P.A. // Drug Discov. Today Technol. 2017. V. 23. P. 27–36.
- Godugu C., Patel A.R., Desai U., Andey T., Sams A., Singh M. // PLoS One. 2013. V. 8. № 1. P. e53708.
- Sokolova E.A., Shilova O.N., Kiseleva D.V., Schulga A.A., Balalaeva I.V., Deyev S.M. // Int. J. Mol. Sci. 2019. V. 20. № 10. Р. 2399. doi: 10.3390/ijms20102399.
- Proshkina G.M., Kiseleva D.V., Shilova O.N., Ryabova A.V., Shramova E.I., Stremovskiy O.A., Deyev S.M. // Mol. Biol. 2017. V. 51. № 6. P. 865–873.
- Mosmann T. // J. Immunol. Methods. 1983. V. 65. № 1–2. P. 55–63.
- Zdobnova T., Sokolova E., Stremovskiy O., Karpenko D., Telford W., Turchin I., Balalaeva I., Deyev S. // Oncotarget. 2015. V. 6. № 31. P. 30919–30928.
- Shcherbo D., Merzlyak E.M., Chepurnykh T.V., Fradkov A.F., Ermakova G.V., Solovieva E.A., Lukyanov K.A., Bogdanova E.A., Zaraisky A.G., Lukyanov S., et al. // Nat. Methods. 2007. V. 4. № 9. P. 741–746.
- Shin S., Ikram M., Subhan F., Kang H.Y., Lim Y., Lee R., Jin S., Jeong Y.H., Kwak J.-Y., Na Y.-J., et al. // RSC Adv. 2016. V. 6. № 52. P. 46952–46965.
- Tang Y., Liu J., Chen Y. // Microelectron. Eng. 2016. V. 158. P. 41–45.
- Nicoletti I., Migliorati G., Pagliacci M.C., Grignani F., Riccardi C. // J. Immunol. Methods. 1991. V. 139. № 2. P. 271–279.
- Arndt-Jovin D.J., Jovin T.M. // J. Histochem. Cytochem. 1977. V. 25. № 7. P. 585–589.
- Purschke M., Rubio N., Held K.D., Redmond R.W. // Photochem. Photobiol. Sci. 2010. V. 9. № 12. P. 1634–1639.
- Krishnamurti U., Silverman J.F. // Adv. Anat. Pathol. 2014. V. 21. № 2. P. 100–107.
- Carlsson J., Nordgren H., Sjöström J., Wester K., Villman K., Bengtsson N.O., Ostenstad B., Lundqvist H., Blomqvist C. // Br. J. Cancer. 2004. V. 90. № 12. P. 2344–2348.
- Murphy C.G., Modi S. // Biologics. 2009. V. 3. P. 289–301.
- Iqbal N., Iqbal N. // Mol. Biol. Int. 2014. V. 2014. P. 852748.
- Mitri Z., Constantine T., O’Regan R. // Chemother. Res. Pract. 2012. V. 2012. P. 743193.
- Stepanov A.V., Belogurov A.A., Ponomarenko N.A., Stremovskiy O.A., Kozlov L.V., Bichucher A.M., Dmitriev S.E., Smirnov I.V., Shamborant O.G., Balabashin D.S., et al. // PLoS One. 2011. V. 6. № 6. P. e20991.
- Pastan I., Hassan R., FitzGerald D.J., Kreitman R.J. // Annu. Rev. Med. 2007. V. 58. P. 221–237.
- Boersma Y.L., Plückthun A. // Curr. Opin. Biotechnol. 2011. V. 22. № 6. P. 849–857.
- Dreier B., Honegger A., Hess C., Nagy-Davidescu G., Mittl P.R.E., Grütter M.G., Belousova N., Mikheeva G., Krasnykh V., Plückthun A. // Proc. Natl. Acad. Sci. USA. 2013. V. 110. № 10. P. E869–877.
- Plückthun A. // Annu. Rev. Pharmacol. Toxicol. 2015. V. 55. P. 489–511.
- de Dios-Figueroa G.T., Aguilera-Marquez J.D.R., Camacho-Villegas T.A., Lugo-Fabres P.H. // Biomedicines. 2021. V. 9. № 6. Р. 602. doi: 10.3390/biomedicines9060602.
- Jensen C., Teng Y. // Front. Mol. Biosci. 2020. V. 7. P. 33.
- Nakayama Y., Takewa Y., Sumikura H., Yamanami M., Matsui Y., Oie T., Kishimoto Y., Arakawa M., Ohmuma K., Tajikawa T., et al. // J. Biomed. Mater. Res. B. 2015. V. 103. № 1. P. 1–11.
- Kun K. // Procedia Eng. 2016. V. 149. № 2. P. 203–211.
- Nicholas P., Rossi G., Williams E., Bennett M., Schork T. // Int. J. Archit. Comput. 2020. V. 18. № 4. P. 371–384.
- Murphy S.V., Atala A. // Nat. Biotechnol. 2014. V. 32. № 8. P. 773–785.
- Wang L., Pumera M. // Trends Analyt. Chem. 2021. V. 135. P. 116151.
- Tolmachev V.M., Chernov V.I., Deyev S.M. // Russ. Chem. Rev. 2022. V. 91. RCR5034. https://doi.org/10.1070/RCR5034
- Shipunova V.O., Deyev S.M. // Acta Naturae. 2022. V. 14. № 1(52). P. 54–72.
Дополнительные файлы