Изменение профиля экспрессии микроРНК в лейкоцитах пациентов с болезнью Паркинсона
- Авторы: Ардаширова Н.С.1, Абрамычева Н.Ю.1, Федотова Е.Ю.1, Иллариошкин С.Н.1
-
Учреждения:
- ФГБНУ «Научный центр неврологии»
- Выпуск: Том 14, № 3 (2022)
- Страницы: 79-84
- Раздел: Экспериментальные статьи
- Дата подачи: 16.05.2022
- Дата принятия к публикации: 04.07.2022
- Дата публикации: 29.10.2022
- URL: https://actanaturae.ru/2075-8251/article/view/11729
- DOI: https://doi.org/10.32607/actanaturae.11729
- ID: 11729
Цитировать
Аннотация
Болезнь Паркинсона (БП) – одно из наиболее распространенных двигательных расстройств, диагностика которого до настоящего времени остается, главным образом, клинической. Для разработки патогенетического лечения БП важна точная диагностика БП на самых ранних стадиях, в связи с чем необходим поиск потенциальных биомаркеров заболевания. Нами оценена диагностическая значимость ряда микроРНК и их взаимосвязь с клиническими характеристиками БП. В исследование включены 70 пациентов с БП и 40 здоровых добровольцев. В лейкоцитах крови оценивали экспрессию 15 микроРНК, отобранных на основании опубликованных данных и современных представлений о молекулярном патогенезе БП. Всем пациентам проведена оценка по клиническим шкалам Hoehn–Yahr, UPDRS, NMSQ, PDQ-39. По результатам исследования выявлено статистически значимое повышение экспрессии miR-7-1-5p, miR-29c-3p и miR-185-5p и снижение экспрессии miR-29a-3p и miR-30c-1-5p в лейкоцитах при БП. Однако показано, что измененный профиль микроРНК обладает умеренной диагностической значимостью. Изменения экспрессии микроРНК были ассоциированы с моторными и немоторными фенотипическими особенностями БП и изменялись на фоне приема противопаркинсонических препаратов. Также показана связь ряда изученных микроРНК с длительностью и тяжестью БП, что потенциально может использоваться в мониторировании прогрессирования заболевания.
Ключевые слова
Полный текст
СПИСОК СОКРАЩЕНИЙ БП – болезнь Паркинсона; REM-фаза – фаза быстрых движений глаз (rapid eye movement); UPDRS – унифицированная рейтинговая шкала оценки болезни Паркинсона (Unified Parkinson’s Disease Rating Scale); NMSQ – опросник немоторных симптомов (Non-Motor Symptoms Questionnaire); HADS – госпитальная шкала тревоги и депрессии (Hospital Anxiety and Depression Scale); MоCA – Монреальская шкала когнитивной оценки (Montreal Cognitive Assessment); PDQ-39 – опросник качества жизни пациентов с болезнью Паркинсона (Parkinson’s Disease Questionnaire).
ВВЕДЕНИЕ
Болезнь Паркинсона (БП) – одно из наиболее распространенных двигательных расстройств, представляющее серьезную медицинскую и социальную проблему. Согласно современным представлениям, БП относится к синуклеинопатиям – заболеваниям, которые характеризуются формированием патологических агрегатов альфа-синуклеина в центральной и периферической нервной системе [1]. К синуклеинопатиям относятся, помимо БП, деменция с тельцами Леви, мультисистемная атрофия, изолированная вегетативная недостаточность. Важным предиктором развития синуклеинопатий является нарушение поведения в REM-фазу сна [1].
Диагностика БП до настоящего времени остается, в первую очередь, клинической. При этом по данным патоморфологической верификации даже специалисты в области двигательных расстройств ставят правильный клинический диагноз БП лишь примерно в 80% случаев [2]. Существующие методы радиоизотопной нейровизуализации (позитронно-эмиссионная и однофотонно-эмиссионная компьютерная томография) позволяют точно оценить состояние дофаминергических проводящих путей и тем самым значительно улучшить точность диагностики БП [3]. Однако это дорогостоящие методы, связанные с лучевой нагрузкой, и они не позволяют дифференцировать БП с синдромами атипичного паркинсонизма [4]. Недостаточная точность прижизненной диагностики, особенно на ранних стадиях заболевания, считается одной из важных причин неудач в испытаниях препаратов для патогенетического лечения БП [5]. Таким образом, весьма актуальна разработка информативных и доступных диагностических биомаркеров БП.
Молекулярный патогенез БП носит сложный характер. Одним из его компонентов предположительно является нарушение эпигенетической регуляции экспрессии генов, в том числе с участием микроРНК [6]. На данный момент в геноме человека выявлено более 5000 различных микроРНК (http://www.mirbase.org). Изученный механизм действия микроРНК заключается в реализации РНК-сайленсинга. В составе РНК-индуцируемого комплекса сайленсинга (RISK) микроРНК связывается с 3’-концом комплементарной мРНК, что приводит к ее деградации и предотвращению трансляции белка [7]. Описаны и другие механизмы регуляции экспрессии с участием микроРНК [8]. Немаловажно, что одна микроРНК может связываться более чем с 200 различными мРНК, индуцируя таким образом сдвиги в регуляции целых белковых ансамблей [9]. Подобные изменения могут быть основой для развития самых разнообразных патологических процессов, в том числе, приводящих к нейродегенерации.
При БП сдвиги концентраций микроРНК, определяемых в крови, могут в значительной степени отражать вовлечение в патологический процесс множества органов и систем – именно с полиорганной патологией связывают развитие столь характерных для БП немоторных проявлений (желудочно-кишечных, кардиальных и др.). Таким образом, знание особенностей концентраций микроРНК в крови позволило бы создать новый информативный биомаркер БП, в том числе для ранней и дифференциальной диагностики заболевания, прогнозирования характера его течения, более точной оценки соотношения моторных и немоторных проявлений и т.д.
Изучена возможность использования тех или иных микроРНК в диагностике БП [10–12]. В некоторых работах в качестве биомаркера БП изучали панели из нескольких микроРНК [13–16]. При этом следует учитывать, что профиль микроРНК достаточно динамичен и подвержен изменениям под воздействием различных факторов. Так, показано, что на профиль микроРНК влияет текущая противопаркинсоническая терапия [17–20] и проводимая пациенту глубинная стимуляция мозга [21]. По результатам анализа опубликованных данных мы выбрали 15 микроРНК, экспрессия которых в крови и головном мозге пациентов с БП значимо отличалась от экспрессии в контрольной группе, как минимум, в двух исследованиях.
В нашей работе оценена значимость выбранных микроРНК для диагностики БП и их взаимосвязь с клиническими характеристиками заболевания.
ЭКСПЕРИМЕНТАЛЬНАЯ ЧАСТЬ
В исследование были включены 70 пациентов с БП и 40 здоровых добровольцев. Группа БП состояла из 35 мужчин и 35 женщин (средний возраст 60.5 ± 11.8 лет). Пациенты контрольной группы были сопоставимы по полу и возрасту с основной группой. Проведение исследования одобрено локальным этическим комитетом Научного центра неврологии, все участники исследования подписывали информированное согласие.
Диагноз БП устанавливали в соответствии с критериями Международного общества по болезни Паркинсона и расстройствам движений – MDS [22]. Возраст дебюта – 53 ± 13 лет, длительность заболевания 6.4 ± 7.0 лет. Смешанная форма БП отмечена у 52 пациентов (74.3%), акинетико-ригидная форма – у 18 (25.7%). Средняя оценка выраженности клинических проявлений по унифицированной рейтинговой шкале оценки болезни Паркинсона (UPDRS) составила 65.6 ± 27.1 балла, средняя стадия заболевания по функциональной шкале Hoehn–Yahr – 2.4 ± 0.9.
Все пациенты заполняли опросник немоторных симптомов – NMSQ; средняя сумма баллов составила 9.0 ± 5.2. Проведено тестирование по госпитальной шкале тревоги и депрессии – HADS (средняя сумма баллов 6.4 ± 4.0 и 7.0 ± 4.6 для тревоги и депрессии соответственно), а также по Монреальской шкале когнитивной оценки – MoCA (23.1 ± 4.2 балла). Пациенты заполняли опросник качества жизни для пациентов с болезнью Паркинсона – PDQ-39 (44 ± 30 баллов).
Большинство пациентов с БП получали противопаркинсонические препараты, в том числе: леводопу (41 пациент, 58.6%), агонисты дофаминовых рецепторов (30 пациентов, 42.6%), препараты амантадина (20, 28.6%). Двадцать три пациента (32.9%) не получали какой-либо терапии на момент включения в исследование.
В работе исследованы следующие 15 микроРНК: miR-7-1-5p, miR-24-1-3p, miR-29a-3p, miR-29c-3p, miR-30c-1-5p, miR-106a-5p, miR-126-3p, miR-129-1-5p, miR-132-3p, miR-135b-5p, miR-146a-5p, miR-185-5p, miR-214-3p, miR-221-3p, miR-520d-5p.
Из венозной крови всех обследуемых выделяли лейкоцитарную фракцию. Далее с помощью набора для выделения РНК RNeasy mini kit (Qiagen) выделяли тотальную РНК по стандартному протоколу производителя. После выделения РНК проводили специфичную для каждой микроРНК обратную транскрипцию с использованием праймеров stem-loop и набора для обратной транскрипции («Синтол»). Относительную концентрацию каждой РНК определяли при проведении полимеразной цепной реакции в реальном времени с помощью соответствующего набора (ООО «Синтол»), в качестве референсной РНК использовали miR-191-5p. Концентрацию РНК рассчитывали по методу 2(-ΔΔC(T)).
Статистическую обработку проводили в программе IBM SPSS и Statistica 10.0. Нормальность распределения значений проверяли с помощью теста Шапиро–Уилка. В связи с тем, что распределение значений микроРНК не соответствовало нормальному, использовали непараметрические критерии: критерий Манна–Уитни, критерий Краскила–Уоллиса, коэффициент корреляции Спирмена. Также использовали логистический регрессионный анализ и ROC-анализ. Статистический уровень значимости принимали равным 0.05.
РЕЗУЛЬТАТЫ
В группе БП по сравнению с контрольной группой выявлено статистически значимое повышение уровня экспрессии трех микроРНК – miR-7-1-5p, miR-29c-3p и miR-185-5p, и снижение экспрессии двух микроРНК – miR-29a-3p и miR-30c-1-5p (табл. 1). Однако, несмотря на статистическую значимость выявленных различий, наблюдалось значительное перекрывание значений относительной экспрессии в исследованных группах.
Таблица 1. Экспрессия микроРНК у пациентов с болезнью Паркинсона и в контрольной группе
МикроРНК | Болезнь Паркинсона | Контрольная группа | р (U) |
miR-7-1-5p | 0.68 [0.19; 1.7] | 0.2 [0.04; 1.5] | 0.024* |
miR-24-1-3p | 455.72 [0.43; 654.6] | 480.88 [0.83; 602.4] | 0.684 |
miR-29a-3p | 0.63 [0.41; 1.01] | 0.97 [0.66; 1.4] | 0.003** |
miR-29c-3p | 1.76 [0.93; 3.58] | 0.77 [0.59; 1.98] | 0.003** |
miR-30c-1-5p | 0.53 [0.34; 1.43] | 1.03 [0.46; 1.77] | 0.043* |
miR-106a-5p | 1.41 [0.43; 3.5] | 1.39 [0.76; 2.8] | 0.691 |
miR-126-3p | 0.23 [0.15; 0.44] | 0.4 [0.11; 0.8] | 0.194 |
miR-129-1-5p | 0.47 [0.2; 2.21] | 0.4 [0.23; 0.71] | 0.403 |
miR-132-3p | 1.01 [0.4; 2.01] | 0.87 [0.37; 1.39] | 0.209 |
miR-135b-5p | 54.5 [4.02; 2479.78] | 284.29 [1.02; 149791.83] | 0.946 |
miR-146a-5p | 0.11 [0.03; 1.37] | 0.07 [0.03; 0.34] | 0.337 |
miR-185-5p | 13631.02 [380.56; 21875.07] | 863.02 [0.17; 14684.43] | 0.017* |
miR-214-3p | 15.23 [6.97; 22.65] | 15.75 [6.01; 27.3] | 0.709 |
miR-221-3p | 0.63 [0.42; 1.04] | 0.72 [0.49; 0.99] | 0.443 |
miR-520d-5p | 0.27 [0.05; 1.02] | 0.52 [0.04; 1.77] | 0.374 |
*р<0.05; **р < 0.01. Жирным шрифтом выделены все случаи, где p<0.05.
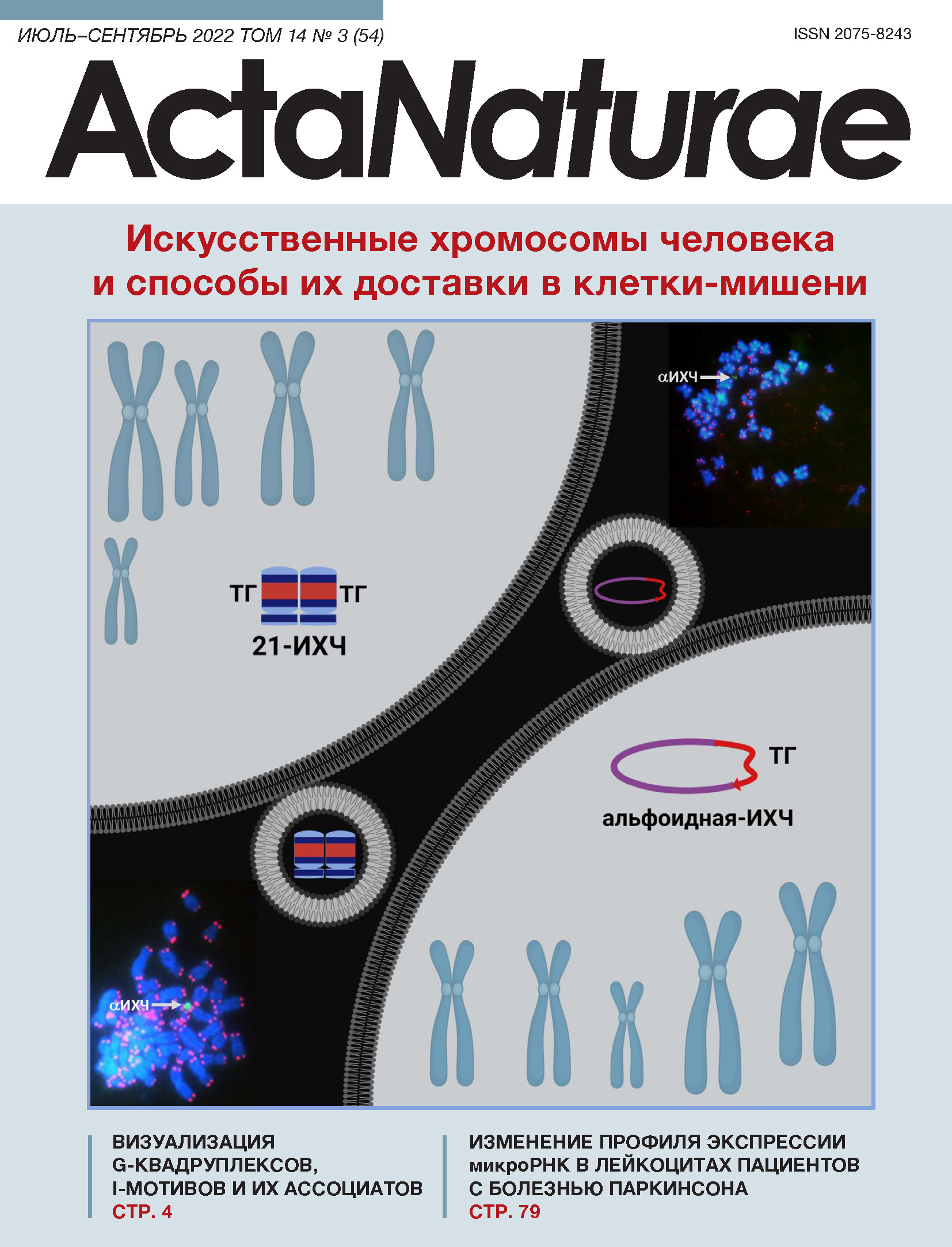
Далее оценили возможность использования отдельных микроРНК в качестве биомаркеров БП. При проведении ROC-анализа установили, что некоторые микроРНК позволяют дифференцировать БП от контроля: miR-7-1-5p (AUC = 0.63, p = 0.024; 95% CI 0.517–0.742), miR-185-5p (AUC = 0.638; p = 0.016; 95% CI 0.53–0.744), miR-29c-3p (AUC = 0.673; p = 0.003; 95% CI 0.56–0.778). Однако очевидно, что чувствительность и специфичность этих биомаркеров недостаточны для применения в диагностике БП. Для поиска наиболее оптимальной комбинации микроРНК, которая могла иметь наибольшую информативность в качестве биомаркера, использовали логистический регрессионный анализ с помощью обратного метода Вальда. Наиболее информативной оказалась комбинация miR-29c-3p и miR-185-5p. При последующем проведении ROC-анализа площадь под кривой составила 0.715 (рис. 1). Таким образом, данная модель с двумя микроРНК позволяет с вероятностью 71.5% дифференцировать пациентов с БП от здоровых лиц.
Рис. 1. ROC-анализ модели логистической регрессии с miR-29c-3p и miR-185-5p для диагностики болезни Паркинсона
Нами изучена взаимосвязь экспрессии микроРНК с клиническими характеристиками БП. Не выявлено значимых корреляций уровней микроРНК с возрастом дебюта, тогда как выявлена одна корреляционная связь слабой силы (R < |0.3|) возраста на момент исследования с miR-135b-5p. Исследование корреляций уровней микроРНК с длительностью заболевания выявило шесть слабых, но значимых корреляций (miR-132-3p, miR-146a-5p, miR-106a-5p, miR-24-1-3p, miR-29a-3p, miR-30c-1-5p), а также две корреляции умеренной силы – с miR-126-3p (R = 0.316; p = 0.07) и miR-129-1-5p (R = 0.385; p = 0.001). Указанные микроРНК могут служить маркерами прогрессирования заболевания.
Анализ экспрессии микроРНК при разных формах БП показал, что при акинетико-ригидной форме уровень miR-29a-3p был значимо выше, чем при смешанной форме – 1.06 [0.6; 1.59] и 0.6 [0.43; 0.85] (p = 0.018) соответственно. Выявлена отрицательная корреляция между уровнем miR-30c-1-5p и стадией заболевания по шкале Hoehn–Yahr (R = –0.303; p = 0.19). При этом обнаружена дифференциальная экспрессия обеих указанных микроРНК (см. табл. 1) при БП и в контрольной группе. Корреляции уровней микроРНК с суммой баллов по шкале UPDRS и ее подшкалами не обнаружено. Выявлена отрицательная корреляция уровня miR-106a-5p с суммой баллов по шкале немоторных симптомов NMSQ (R = –0.358, p = 0.011). Не выявлено корреляций с баллами по шкалам тревоги и депрессии HADS. Корреляций с выраженностью когнитивных нарушений по шкале МоСА также не найдено.
Экспрессия miR-29a-3p (p = 0.045) была статистически значимо снижена в группе пациентов, которые получали терапию леводопой, у пациентов, принимавших как агонисты дофаминовых рецепторов, так и амантадин, наблюдалось снижение miR-7-1-5p (p = 0.0048 и р = 0.037 соответственно). Интересно, что экспрессия и miR-7-1-5p, и miR-29a-3p при БП отличается от экспрессии в контрольной группе (см. табл. 1).
ОБСУЖДЕНИЕ
В настоящее время проведено значительное количество исследований биомаркерной роли микроРНК при БП, однако их результаты во многом противоречивы: это связано с тем, что разные исследователи изучают разные компоненты крови (плазма, лейкоциты, сыворотка, везикулы), а также с большим разнообразием изучаемых микроРНК и различиями в методах их детекции [23].
В настоящей работе мы использовали 15 микроРНК, экспрессия которых при БП, как показано в предшествующих исследованиях, значимо отличалась от экспрессии в контроле. По нашим данным, наибольшей диагностической значимостью при БП обладает комбинация двух микроРНК – miR-29c-3p и miR-185-5p. Отмечено также значимое повышение уровня miR-7-1-5p и снижение miR-29а-3p при БП, однако на уровень этих микроРНК, как показано в нашей работе, существенно влияет противопаркинсоническая терапия. Кроме того, показано значимое снижение miR-30c-1 при БП. Уровень этой микроРНК неуклонно снижается по мере течения болезни и нарастания ее тяжести по функциональной шкале Hoehn–Yahr, поэтому он может использоваться как маркер прогрессирования заболевания (т.е. маркер развернутых стадий БП).
Ряд других микроРНК, уровень которых был таким же, как в контрольной группе, тем не менее оказался связанным с немоторными проявлениями БП (miR-106a-5p) и с длительностью заболевания (miR-126-3p, miR-129-1-5p). Таким образом, эти микроРНК, не являясь биомаркерами непосредственно заболевания, могут быть полезными для более точного определения немоторных фенотипов БП и более объективного мониторинга течения болезни.
Роль miR-185 при БП анализировали в нескольких работах. На обработанной MPTP культуре дофаминергических клеток нейробластомы SH-SY5Y показано снижение уровня miR-185, а повышение экспрессии miR-185 уменьшало MPTP-индуцированный апоптоз и аутофагию [24]. В работе Rahimmi и соавт. на культурах клеток SH-SY5Y и крысах линии Wistar, у которых паркинсонизм вызывали с помощью инъекций ротенона, показано, что ингибирование экспрессии miR-185 специально подобранной малой интерферирующей РНК приводит к значительному повышению экспрессии гена LRRK2. Этот ген играет важную роль в патогенезе БП: мутации в нем приводят к развитию наследственных форм БП [25]. На животных моделях показано снижение miR-185 и увеличение экспрессии LRRK2 в черной субстанции и стриатуме. В работе Briggs и соавт. также наблюдали изменение экспрессии miR-185 в черной субстанции, но в противоположном направлении [26]. Возможность использования miR-185 в качестве биомаркера изучали в нескольких работах и в двух из них выявили снижение экспрессии уровня этой микроРНК при БП по сравнению с контрольной группой [15, 27], тогда как в нашей работе обнаружено повышение экспрессии данного потенциального маркера. Таким образом, результаты определения уровня экспрессии miR-185 при БП остаются противоречивыми.
Семейство miR-29 состоит из трех микроРНК: miR-29a, miR-29b и miR-29с. При изучении использования этих микроРНК в качестве биомаркеров неоднократно наблюдали снижение экспрессии miR-29a и miR-29c в крови пациентов с БП, причем снижение уровня miR-29a и miR-29c нарастало по мере прогрессирования заболевания по шкале Hoehn–Yahr [28]. В проспективном исследовании пациентов группы риска синуклеинопатий – пациентов с нарушениями поведения в REM-фазу сна, которым впоследствии установлен диагноз синуклеинопатии, выявлено снижение уровней miR-29a и miR-29c [29]. Отдельно miR-29a изучали в нескольких работах и показали снижение ее уровня, что соответствует нашим результатам [14, 30, 31]. Serafin и соавт. описали повышение экспрессии miR-29a только у пациентов, получающих терапию леводопой, но не выявили изменений у пациентов, не получавших лечения [19]. В нашей работе также показано снижение уровня miR-29a при назначении препаратов леводопы.
Увеличение экспрессии miR-29c, обнаруженное у пациентов с БП в турецкой популяции [32], соответствует нашим результатам, но противоречит большинству имеющихся данных [12, 14, 31]. В число мишеней этого весьма перспективного с патогенетической точки зрения семейства микроРНК входят выявленные с помощью предсказательных алгоритмов мРНК гена PARK-7 (DJ-1), мутации в котором могут приводить к развитию БП, мРНК GPR37, субстратом которой является белок паркин, ассоциированный с развитием ранней БП, а также различные регуляторы процессов апоптоза (Puma, Bim, Bak, Bcl2, IGF1, AKT1). Мишени отдельных микроРНК семейства miR-29 могут значительно перекрываться, но их роль в патогенезе различных форм БП не вызывает сомнений.
Согласно имеющимся данным, miR-7 снижает экспрессию альфа-синуклеина [33, 34], нарушение процессинга которого считается одним из ключевых звеньев патогенеза БП. В одной из работ показано снижение экспрессии miR-7 в головном мозге пациентов с БП, за счет чего, вероятно, увеличивается экспрессия альфа-синуклеина [6]. Показано также, что снижение экспрессии miR-7 увеличивает вероятность апоптоза и ухудшает рост дофаминергических нейронов в культуре [35]. В нашей работе, наоборот, уровень экспрессии miR-7 в группе БП был значимо выше, чем в контроле. В работе Alieva и соавт. также показано многократное увеличение экспрессии miR-7 в подгруппе пациентов с БП, получающих противопаркинсонические препараты [18]. В нашей работе не отмечено влияния леводопа-терапии на уровень miR-7, тогда как назначение агонистов дофаминовых рецепторов и амантадинов ассоциировано со снижением экспрессии miR-7. Противоречивые результаты в отношении уровня miR-7 при БП и влияния на него противопаркинсонической терапии требуют дальнейших уточнений.
Снижение уровня miR-30c-1 при БП, описанное в работах Vallelunga и соавт. и Martins и соавт., соответствует полученным нами результатам [31, 36]. Не установлено прямого влияния miR-30c-1 на экспрессию генов, ответственных за развитие БП, однако с помощью различных баз данных показано, что предполагаемые мишени данной микроРНК (Notch1, HDAC4, BECN1, UBE2I, HSPA4 и DNMT1) играют роль в регуляции аутофагии и апоптоза дофаминергических клеток [37].
ЗАКЛЮЧЕНИЕ
Таким образом, нами показано, что комбинация двух микроРНК (miR-29c-3p и miR-185-5p) может рассматриваться как потенциальный биомаркер БП, хотя и с умеренной диагностической значимостью. Показано, что уровень экспрессии ряда микроРНК отражает клинические характеристики БП, изменяется с длительностью и стадией заболевания, а также под воздействием проводимой терапии, может быть маркером формы заболевания и связан с выраженностью немоторных проявлений и качеством жизни пациентов с БП. Согласно опубликованным данным, некоторые из диагностических микроРНК связаны с определенными звеньями патогенеза БП. Полученные нами результаты являются предварительными и требуют дальнейших исследований.
Об авторах
Наталья Сергеевна Ардаширова
ФГБНУ «Научный центр неврологии»
Автор, ответственный за переписку.
Email: ardashirova.n@yandex.ru
ORCID iD: 0000-0002-4813-9912
аспирант
Россия, Москва, 125367Наталья Юрьевна Абрамычева
ФГБНУ «Научный центр неврологии»
Email: nataabr@rambler.ru
руководитель ДНК-лаборатории 5-ого неврологического отделения, к.б.н.
Россия, Москва, 125367Екатерина Юрьевна Федотова
ФГБНУ «Научный центр неврологии»
Email: ekfedotova@gmail.com
руководитель 5-ого неврологического отделения, д.м.н.
Россия, Москва, 125367Сергей Николаевич Иллариошкин
ФГБНУ «Научный центр неврологии»
Email: snillario@gmail.com
заместитель директора по научной работе, директор Института мозга, д.м.н., проф., чл.-корр. РАН
Россия, Москва, 125367Список литературы
- Coon E.A., Singer W. // CONTINUUM: Lifelong Learning in Neurology. 2020. V. 26. № 1. P. 72–92.
- Rizzo G., Copetti M., Arcuti S., Martino D., Fontana A., Logroscino G. // Neurology. 2016. V. 86. № 6. P. 566–576.
- Gerasimou G., Costa D.C., Papanastasiou E., Bostanjiopoulou S., Arnaoutoglou M., Moralidis E., Aggelopoulou T. Gotzamani-Psarrakou A. // Ann. Nucl. Med. Japan. 2012. V. 26. № 4. P. 337–344.
- Arena J.E., Stoessl A.J. // Parkinsonism and Related Disorders. 2016. V. 22. P. S47–S51.
- Lang A.E., Espay A.J. // Movement Disorders. 2018. V. 33. № 5. P. 660–677.
- Tatura R., Kraus T., Giese A., Arzberger T., Bucholz M., Höglinger G., Muller U. // Parkinsonism and Related Disorders. 2016. V. 33. P. 115–121.
- Wahid F., Shehzad A., Khan T., Kim Y.Y. // Biochim. Biophys. Acta – Mol. Cell Res. 2010. V. 1803. № 11. P. 1231–1243.
- Mathonnet G., Fabian M.R., Svitkin Y.V., Parsyan A., Huck L., Murata T., Biffo S., Merrick W., Darzynkiewicz E., Pillai R.S., et al. // Science. 2007. V. 317. № 5845. P. 1764–1767.
- Leggio L., Vivareli S., L’Episcopo F., Tirolo C., Caniglia S., Testa N., Barchetti B., Iraci N. // Int. J. Mol. Sci. 2017. V. 18. P. 2698.
- Ma F., Zhang X., Yin K.-J. // Exp. Neurol. 2020. V. 323. P. 113094.
- Cao X., Lu J.-M., Zhao Z.-Q., Li M.-C., Lu T., An X.-S., Xue L.-J. // Neurosci. Lett. 2017. V. 644. P. 94–99.
- Ma W., Li Y., Wang C., Xu F., Wang M., Liu Y. // Cell. Biochem. Funct. 2016. V. 34. P. 511–515.
- Kean S., Petillo D., Kang U.J., Resau J.H., Berryhill B., Linder J., Forsgren L., Neuman L.A., Tan A.C. // J. Parkinson’s Dis. 2012. V. 2. P. 321–331.
- Botta-orfila T., Morato X., Compta Y., Lozano J.J., Falgas N., Valldeoriola F., Pont-Sunyer C., Vilas D., Mengual L., Fernandez M., et al. // J. Neurosci. Res. 2014. V. 92. № 8. P. 1–7.
- Ding H., Huang Z., Chen M., Wang C., Chen X., Chen J., Zhang J.// Parkinsonism Related Disorders J. 2016. V. 22. P. 68–73.
- Dong H., Wang C., Lu S., Yu C., Huang L., Feng W., Xu H., Chen X., Zen K., Yan Q., et al. // Biomarkers. 2016. V. 21. № 2. P. 129–137.
- Margis R.R., Margis R.R., Rieder C.R.M. // J. Biotechnol. 2011. V. 152. № 3. P. 96–101.
- Alieva A., Filatova E.V., Karabanov A.V., Illarioshkin S.N., Limborska S.A., Shadrina M.I., Slominsky P.A. // Parkinsonism Related Disorders J. 2014. V. 21. № 1. P. 14–16.
- Serafin A.., Foco L., Zanigni S., Blankenburg H., Picard A., Zanon A., Gianni G., Pichler I., Maurizio F.F., Cortell P., Pramstaller P.P., Hicks A.A., Domingues F.S., Schwienbacher C. // Neurology. 2015. V. 84. P. 1–9.
- Caggiu E., Paulus K., Mameli G., Arru G., Sechi G.P., Sechi L.A. // eNeurologicalSci. 2018. V. 13. P. 1–4.
- Soreq L., Salomonis N., Bronstein M., Greenberg D.S., Israel Z., Bergman H., Soreg H.// Front. Mol. Neurosci. 2013. V. 6. P. 1–20.
- Postuma R., Berg D., Stern M., Poewe W., Olanow C.W., Oertel W., Obeso J., Marek K., Litvan I., Lang A., et al. // Mov. Disord: Official J. Mov. Disord. Soc. 2015. V. 30. № 12. P. 1591–1601.
- Nies Y.H., Mohamad Najib N.H., Lim W.L., Kamaruzzaman M.A., Yahaya M.F., Teoh S.L.// Front. Neurosci. 2021. V. 15. P. 660379.
- Wen Z., Zhang J., Tang P., Tu N., Wang K., Wu G. // Mol. Med. Rep. 2018. V. 17. № 1. P. 131–137.
- Rahimmi A., Peluso I., Rajabi A., Hassanzadeh K. // Oxid. Med. Cell. Longev. Hindawi. 2019. V. 2019. P. 5019815.
- Briggs C.E., Wang Y., Kong B., Woo T.U., Iyer L.K., Sonntag K.C. // Brain Res. 2015. V. 1618. P. 111–121.
- Chen L., Yu Z. // Brain Behav. 2018. V. 8. № 4. P. e00941.
- Bai X., Tang Y., Yu M., Wu L., Liu F., Ni J., Wang Z., Wang J., Fei J., Wang W., et al.// Sci. Rep. 2017. V. 7. № 1. P. 5411.
- Fernández-Santiago R., Iranzo A., Gaig C., Serradell M., Fernández M., Tolosa E., Santamaría J., Ezquerra M. // Ann. Neurol. 2015. V. 77. № 5. P. 895–901.
- Barbagallo C., Mostile G., Baglieri G., Giunta F., Luca A., Raciti L., Zappia M., Purrello M., Ragusa M., Nicoletti A. // Cell. Mol. Neurobiol. 2020. V. 40. № 4. P. 531–546.
- Martins M., Rosa A., Guedes L.C., Fonseca B.V., Gotovac K., Violante S., Mestre T., Coelho M., Rosa M.M., Martin E.R., et al. // PLoS One. 2011. V. 6. № 10. P. e25443.
- Ozdilek B., Demircan B. // Int. J. Neurosci. 2020. V. 131. № 12. P. 1181–1189.
- Doxakis E. // J. Biol. Chem. 2010. V. 285. № 17. P. 12726–12734.
- Junn E., Lee K.W., Jeong B.S., Chan T.W., Im J.Y., Mouradian M.M. // Proc. Natl. Acad. Sci. USA. 2009. V. 106. № 31. P. 13052.
- Li S. Lv X., Zhai K., Xu R., Zhang Y., Zhao S., Qin X., Yin L., Lou J.// Am. J. Transl. Res. 2016. V. 8. № 2. P. 993–1004.
- Vallelunga A., Ragusa M., Di Mauro S., Iannitti T., Pilleri M., Biundo R., Weis L., Di Pietro C., De Iuliis A., Nicoletti A., et al. // Front. Cell. Neurosci. 2014. V. 8. P. 1–10.
- Vallelunga A., Iannitti T., Dati G., Capece S., Maugeri M., Tocci E., Picillo M., Volpe G., Cozzolino A., Squillante M., et al. // Mol. Biol. Rept. 2019. V. 46. № 2. P. 1661–1666.
Дополнительные файлы